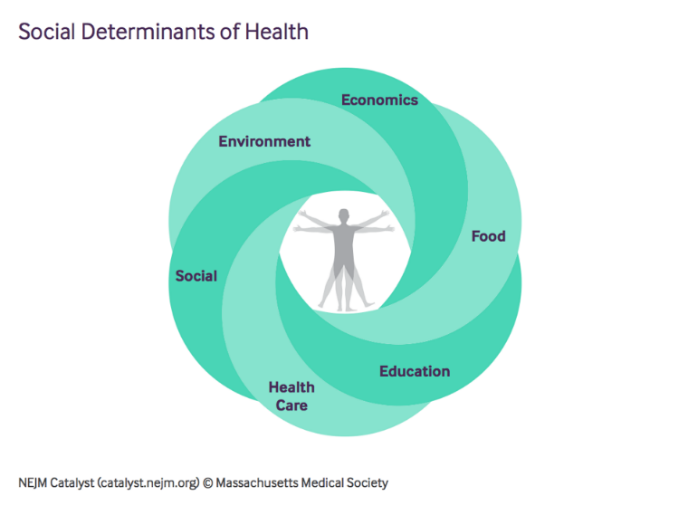
What are Social Determinants of Health?
Economic and social conditions – like stable housing, reliable transportation, and access to healthy foods – have a powerful impact on our health and wellness. Known as social determinants of health, a focus on these non-medical factors has the potential to improve health and well-being and to increase the government’s return on investment in both health and social services programs.

The COVID-19 crisis has dramatically exacerbated these challenges, by creating additional barriers to access, and stretching those organizations seeking to address health and social needs in unprecedented ways. More and more evidence is showing that COVID-19 is disproportionately harming those with underlying health conditions or other risk factors, which are often exacerbated by social determinants. While there are regional pockets of innovation, social service networks, public health organizations, and the health care system are not generally connected in a sustainable, standardized way, which limits data sharing, shared accountability, and service coordination.
Efforts to Address Social Determinants
The federal government directs and supports many programs that seek to address the needs of individuals, including food assistance, housing and supportive housing, transportation, and education and workforce training programs. Programs such as the Supplemental Nutrition Assistance Program (SNAP), run by the US Department of Agriculture, and Continuum of Care (CoC), run by the US Department of Housing and Urban Development (HUD), help to improve health and wellbeing by providing nutrition benefits and support for those experiencing homelessness.
Cross-sector, evidence-based interventions that address social determinants of health hold the potential to improve the health and well-being of Americans and to increase the government’s return on investment in health and social services programs such as Medicaid and Medicare.

Federal, state, and private sector organizations are increasingly looking to deploy social determinants of health interventions to manage costs and improve health outcomes. However, one of the greatest challenges to high-impact interventions is the difficulty in navigating and coordinating the many fragmented programs aimed at addressing health care needs, food insecurity, housing instability, workforce supports, and transportation reliability, among others. Complex program requirements and misaligned incentives across federal, state, local, and non-governmental programs make it hard for states, localities, and Tribes to effectively coordinate, test new approaches, and scale those that work.
Leadership is needed to break down the barriers that impede coordination between health, public health, and social services programs and to encourage the development of sustainable, evidence-based, cross-sector solutions that bridge the gaps and improve outcomes.
How Does this Fit into Health Equity?
According to HHS’ Health Resources and Services Administration:
- Health Equity is the absence of disparities or avoidable differences among socioeconomic and demographic groups or geographical areas in health status and health outcomes such as disease, disability, or mortality.
- Social Determinants of Health are the conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.
Social Determinants of Health factor into health outcomes, and the presence of social determinants may disparities. Therefore, addressing social determinants is an important component of the broader effort to advance health equity.